General Information
What is the urethra?
The urethra is the tube that carries urine from the bladder to the outside of the body.
Its anatomy differs between males and females.
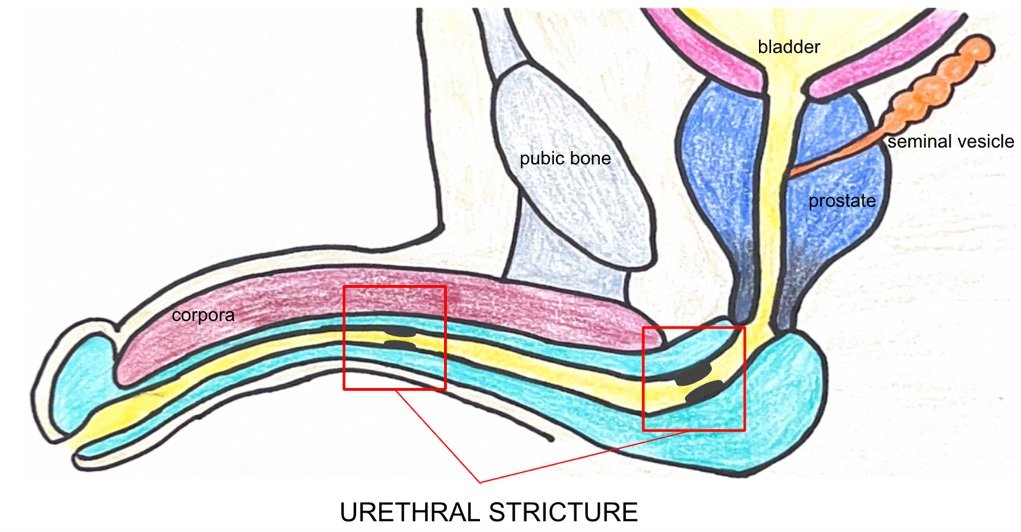
In males, the urethra is long and runs through the prostate, pelvic floor, and penis. The urethral meatus is the opening at the tip of the penis where urine comes out of.
In females, the urethra is shorter and straighter than in males. It runs from the bladder to the urethral meatus, which is located between the clitoris and the vaginal opening.
What is a urethral stricture?
Urethral stricture is a condition where the urethra becomes narrow, making it difficult to pass urine.
It occurs when the tissues in the urethra are damaged or scarred, leading to a constriction or blockage in the urinary tract.
Urethral strictures are much more common in men and are most common in the middle part of the urethra.
Many of these strictures are secondary to prior surgeries of the urinary tract or catheterizations, but up to half of all urethral strictures have an unknown cause.
What are the signs and symptoms of urethral stricture?
The signs and symptoms of urethral stricture may include:
Difficulty passing urine or slowed urine flow.
Frequent urination.
Pain or discomfort during urination.
Recurrent urinary tract infections.
Blood in the urine.
Inability to empty the bladder completely.
Urinary incontinence or leakage.
How is urethral stricture diagnosed?
Uroflow:
This is a diagnostic test used to measure the volume and speed of urine flow during urination.
It is non-invasive and painless. It is done in clinic.
During uroflow, the patient urinates into a special device that measures the amount of urine voided, the time it takes to void the urine, and the speed of the urine flow. The test can also detect any interruptions in the flow of urine, which may indicate a blockage or narrowing of the urethra.
Post-void residual (PVR):
Often done after uroflow, this is a simple ultrasound of the bladder to measure how well you have emptied.
Cystoscopy:
This is a diagnostic procedure used to examine the inside of the bladder and urethra.
During the procedure, the patient lies supine on an examination table. The doctor then inserts a thin, flexible tube called a cystoscope through the urethra and into the bladder. The cystoscope has a light and a camera attached to it, which allows the doctor to see inside the bladder and urethra on a video screen.
What are treatment options for urethral stricture?
There are several treatment options available for urethral stricture, depending on the severity of the condition.
Optilume urethral dilation:
Optilume is the brand name for a type of balloon used for urethral dilation.
It is a minimally invasive procedure that uses a special balloon catheter to dilate the narrowed segment of the urethra. The balloon is coated with a medication called paclitaxel which discourages scar tissue formation.
Optilume urethral dilation is performed on an outpatient basis, typically under local anesthesia or moderate sedation. It does have to happen in the operating room for insurance reasons.
You will have a catheter for 2 days after this procedure.
Urethroplasty:
During this surgery, a small incision is made in the area between the scrotum and the anus.
The urethra is visualized and the area of stricture identified.
Various techniques can be used to widen or reconstruct the urethra so that urine can flow more freely. This may involve removing scar tissue, using grafts from the inside of your cheek or your bottom lip, or other methods depending on the individual case.
You will have a catheter for 2 weeks after this procedure.
Post-Operative Instructions
***DISCLAIMER***
The below instructions are provided to Dr Alford’s patients. If you are undergoing a procedure with a different surgeon, please follow the discharge instructions that were given to you at discharge.
Catheter Care
You will have a catheter in your urethra for 2 weeks after surgery to allow for maximal healing.
Make sure the bag is always below the penis so that it can drain.
You may swap the leg bag for the night bag as needed.
Some blood in the urine is considered normal after this surgery.
Wound Care
You may shower the day after surgery. Do not scrub the incision.
No baths or submersion in water for 2 weeks after surgery.
There may be some bleeding from the sutures. Apply gentle pressure until it stops.
The sutures will dissolve and fall out over the next 2-3 weeks.
If you had an oral mucosal graft taken:
There is a patch sewn into place where the mucosal graft was harvested. The sutures are dissolvable.
It is normal for the graft to begin to lift up as the mucosa heals underneath and the sutures dissolve.
It is normal to have a slight bit of bleeding or discharge from under the graft while your mouth is healing. You may apply gentle pressure to your graft site if you do experience ballooning of the graft or moderate bleeding.
Medications
Tylenol or ibuprofen are fine to take for pain.
You may take oxycodone for breakthrough pain.
You will be prescribed medications to help with bladder spasms. Take these if needed. Stop taking these at least 48 hours before your appointment for catheter removal.
If you had an oral graft taken, magic mouthwash will help your cheek/lip heal after taking the graft.
Diet
Regular diet, as tolerated. It is normal to have a lower appetite after any surgery.
If you had a graft taken from your cheek, chew primarily on the right side of your mouth.
Avoid very hot or very cold foods/liquids for 2 weeks.
Activity
No heavy lifting or strenuous activity/exercise for 2 weeks after surgery.
No baths, swimming pools, or hot tubs until catheter comes out.
No straddle activities (bike riding, horseback riding, motorcycle riding) for 1 month after surgery.
A soon as you feel well enough, you may go back to work.
Post-Operative Follow-up
See your surgeon approximately 2 weeks after surgery for catheter removal.
You will then follow on a regular basis for 1 year after surgery to ensure your stricture does not recur.